Dab Pen (Wax Pen) Vaporizers
Discreet 510 Vape Battery (Concealed)
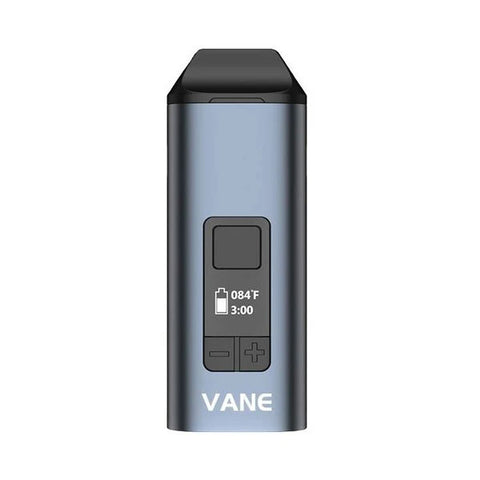
Dry Herb Vaporizers
510 Thread Battery for Carts
Electric Dab Rig
Featured Collections
Welcome to SlickVapes.com!
-

Get Connected 24/7
Do you have any questions? Send it through our contact us and we will get back to you ASAP.
-

Fast & Discreet Shipping
Free shipping on orders above $49.99. Most our orders are shipped same day. We care about your privacy so all our packages come unmarked.
-

Lowest prices guaranteed
We have huge vape sales on all major brands or as much as 50% off vaporizers. Enjoy quality at a discounted price.
-

100% Authentic
All our items are guaranteed 100% Authentic. As an authorized retailer our products are covered by manufactured warranty or better!
-

Great Selection
We hand pick the vapes we offer and choose amongst the winners. We weed out the crap and only offer the best.
SlickVapes.com has been designed and developed for you deal seekers out there. You see everyone has similar prices and offerings, ours are just better. We wanted a shop that you could buy vaporizers at top discounts. All of the vapes we sell are 100% authentic guaranteed! We harness great long-term relationships direct with the manufacturers to offer you better prices and top notch customer service. To make it easy we offer vape deals on our coupon code page that we update daily. We also scatter deals all over the web for the savvy deal finder. Act fast on our deals because once they’re gone who knows when they’ll be back!
👍 New to vaping? We created a guide on how to choose the right vaporizer for you. Whether you’re trying to get better flavor from your herb, dry leaf, and concentrates or just trying to find a stealthier and healthier way to medicate, we’ve got you covered. Our staff has taken the time to test each product in our amazing lines: desktop vaporizers, portable vaporizers, vape pens, dry herb vapes, concentrate vapes, wax vaporizers and dab pens, dabbers, enails, erigs, so we can recommend you a great device that will work for your vaping style! If you have any questions, just ask! Our staff is accessible 24/7. No really, I force them to be available from their phones so you’re sure to hear back from one of us quick. We "weed" out our vapes to give you a great selection to buy from.
Buy discount vaporizers from the top brands! Our device selection is handpicked and quality assured before adding to our list. If we don't like it, you won't see it here! Our most popular high end vaporizers for purchase are: Storz Bickel Mighty / Crafty+ vaporizers, Davinci IQ, Firefly 2+, and the Arizer Solo 2.
Looking for Dab Pens and Electric Dab Rigs? You can't go wrong with Yocan products like the Evolve, Evolve Plus, Kandypens and Puffco for portability. Electronic dab rigs we recommend are the new Focus V Carta Vape Dab Rig, Pulsar Rok, and the new Boost Evo by Dr. Dabber.
Subscribe below to know when we discount some of our best dry herb vaporizers for sale you will be the first to know. For the veteran who wants to use concentrates and wax, we recommend going straight to a vape pen or glass globe atomizers. We offer the cheapest pricing and even discount some of the top vendors. Finding vapes for sale online for the cheapest price can be daunting so if you find another authorized distributor with lower pricing, we'll be happy to price match the item for you.
Make the vaporizer buying experience a good one with Slick Vapes!